SURGERY
Retina and Vitreous Surgery
The retina is the inner lining of the eye. It consists of several layers, including a layer of light-sensitive
cells – rods and cones responsible for the sharpness and color of our vision – which transmit the light
stimulus to the brain via the optic nerve. The retina also contains the area of the sharpest vision, the
macula lutea. The retina is closely connected with the vitreous body, a transparent gel-like substance
that fills the interior of the eye.
Symptoms
Both the retina and vitreous are threatened by changes associated with increasing age. A wide range of diseases affecting these two important structures can be caused by trauma, genetics, or metabolic and systemic conditions. In diabetics, the most common threats are diabetic retinopathy and diabetic macular edema. Other common retinal diseases include macular degeneration (AMD), vascular occlusions, macular holes, epiretinal membranes, and retinal detachment – amotio.
Some diseases progress almost without symptoms, which poses a danger of late diagnosis. Therefore, regular eye check-ups are especially important for diabetics, seniors in general, and people with high myopia, where the doctor can diagnose and catch the disease early. Symptoms indicating a retinal issue, which should not be overlooked or ignored, include:

flashes of light in the eye
dark shadow in the field of vision
dark spots in the field of vision
If you notice any of the following symptoms, immediately see an ophthalmologist or go to an emergency eye clinic.
A diagnosis such as retinal detachment (amotio retinae), in which the retina becomes detached, presents with sudden vision loss – which naturally prompts patients to seek urgent help. You should also be alert if your vision suddenly worsens, as this is a sign that immediate action is needed. It is especially important to recognize the symptoms of retinal detachment, which occur more frequently in patients with high myopia, after eye or head trauma, with degenerative retinal changes, and in advanced stages of diabetes.
Examination Process
We have created a special concept of examinations and measurements for the diagnosis of retinal diseases for our patients. The examinations aimed at assessing the condition of the retina and vitreous include the following measurements:
– visual acuity testing
– fundus examination
– intraocular pressure measurement
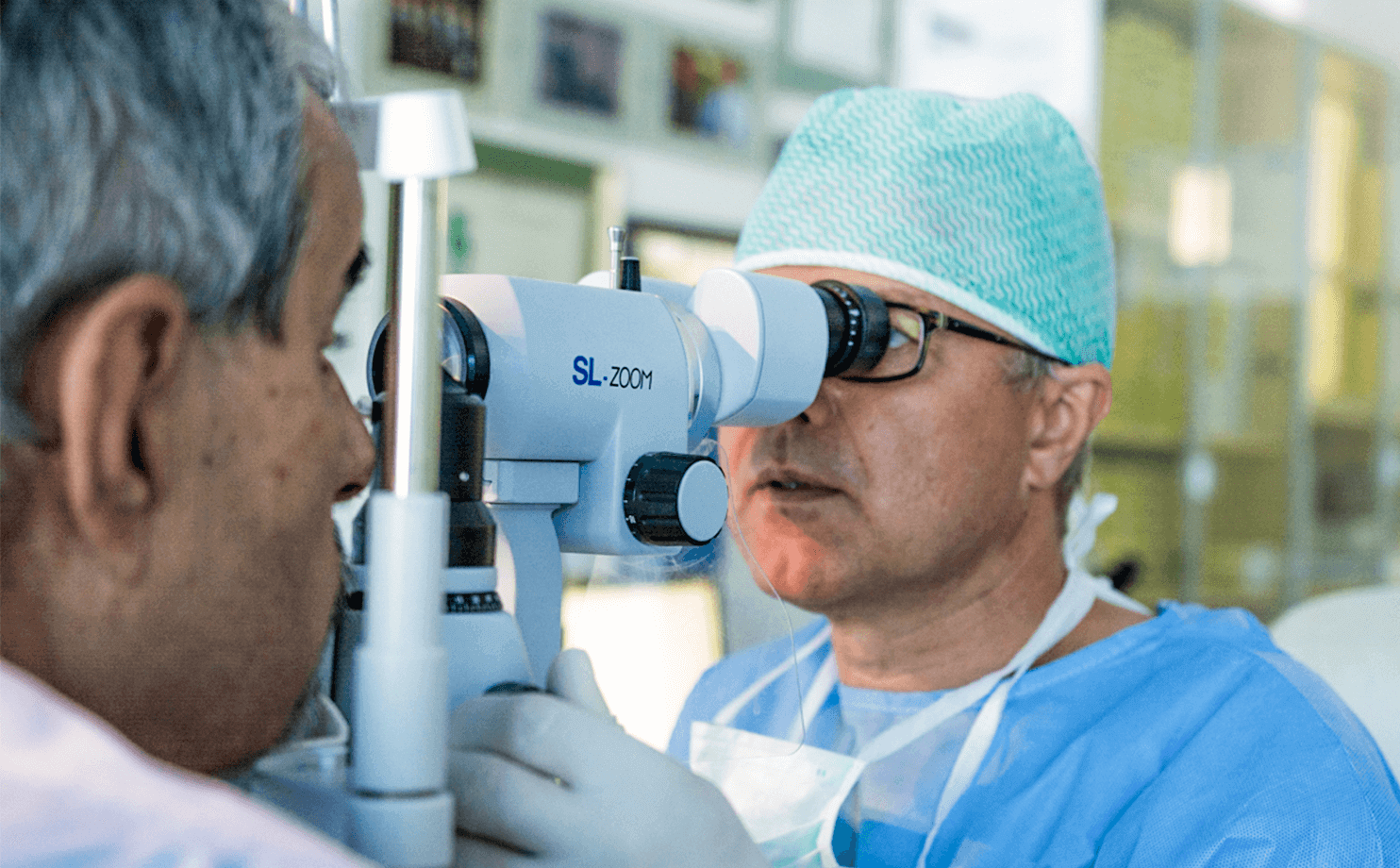
– slit lamp examination
– fundoscopy
– ultrasonography
– perimetry
– OCT examination (Optical Coherence Tomography)
Our retinal specialist will evaluate your condition and, based on that, choose a specific type of treatment.
Surgery
We provide our patients with comprehensive treatment of retinal and vitreous diseases and, as one of the few clinics in Slovakia, we perform retina surgeries within same-day surgery without hospital admission. We carry out laser procedures on the retina, surgical treatments, operate using the globally recognized PPV – Pars Plana Vitrectomy method, and administer biological anti-VEGF treatment.
PPV – Pars Plana Vitrectomy is one of the most demanding eye surgeries and has undergone significant development in recent years. Today, thanks to technological advances and equipment, as well as progress in medical science, it is a micro-invasive outpatient procedure. The entry into the eye is smaller than one millimeter, and the surgeon enters through a place called Pars Plana. Using a surgical instrument called a vitrector, the surgeon accesses the deeper parts of the eye, reaching the retina, where necessary actions are performed depending on the diagnosis. The surgery lasts from 30 minutes to 2 hours, depending on the diagnosis and its condition. After the procedure, the patient goes home. After a week of rest and following the doctor’s instructions at home, patients can return to a full life, depending on the specific diagnosis. The most common diagnoses we treat with the PPV method include:
– Epiretinal membrane – a thin layer of fibrous tissue on the surface of the retina in the macula area,
– AMD – age-related macular degeneration – treated with intraocular anti-VEGF injections,
– Retinal detachment – amotio retinae,
– Macular hole,
– Lamellar macular hole,
– Vitreomacular traction syndrome,
– Vitreous hemorrhage – bleeding into the vitreous,
– Diabetic retinopathy – administration of biological treatment in the form of intraocular anti-VEGF injections and retinal laser coagulation,
– Management of complications during cataract surgery,
– Vitreous opacities – floating particles or bodies of various origin – precipitated hyaluronic acid, cholesterol, remnants of vitreous hemorrhage.
TREATMENT OF MACULAR HOLES
At the Dr. Böhm Eye Center, we also specialize in the treatment of macular holes. Macular holes are located in the center of the sharpest vision of the retina. It is a serious retinal disease that we diagnose in an increasing number of patients every year.
The most common symptoms include:
Distorted vision. Shapes and objects appear deformed, often in the shape of an hourglass.
Vision loss areas. Depending on the hole’s size, the patient perceives central vision loss. For example, while reading, certain letters in a word may disappear. The patient does not see the whole word and must move their head to find the letters.
Treatment using the Lamina Limitans Interna Method
During the procedure, the surgeon removes the vitreous and membranes that are exerting traction on the retina and causing the hole to form. The innermost membrane of the retina (lamina limitans interna) is removed to release the traction forces on the retina. The macular hole closes in 95–98% of patients. In approximately 3–4% of patients, the hole does not close after the first surgery and requires further surgical treatment.
We currently use the most modern membrane peeling techniques, which increase the success rate of macular hole closure.
During the procedure, you can rely on our team of specialists.
MUDr. Peter Böhm Jr. - Cataract & Retina Surgeon
He is the lead retinal surgeon at the eye center and also performs cataract surgeries and treats
complications related to cataract operations.

MUDr. Peter Böhm - Medical Director, Dr. Böhm Eye Center
In addition to performing cataract, retina and vitreous surgeries, he also specializes in the
comprehensive diagnosis and treatment of glaucoma.

Better to book today
We have many satisfied clients and patients waiting.
FREQUENTLY ASKED QUESTIONS
How often should I go for a check-up?
The frequency of check-ups will be determined by your treating ophthalmologist.
“Patients who do not adhere to regular examinations often don’t realize the risks they are taking with such a careless approach. They face the danger of permanent retinal damage and vision loss. However, if check-ups are properly timed, we can preserve vision in the long term. This significantly reduces the risk of complications such as vitreous hemorrhage, tractional retinal detachment, vision loss, or proliferative diabetic retinopathy,” explains Dr. Böhm Sr.
Patients who cooperate well have a significantly lower risk of complications.
What is AMD?
Age-related macular degeneration (of the macula – the area of the sharpest vision) is a condition that most commonly affects patients over the age of 65.
The exact cause of its development is unknown. However, we do know the risk factors. The most significant are age, an unhealthy lifestyle, and genetics. Around the age of 65, the disease occurs in approximately 10% of the population. Over the age of 75, almost every third person suffers from the condition.
AMD also has a genetic basis. Risk factors also include sunlight and exposure to blue light, a lack of antioxidants, and smoking. Several studies confirm that in smokers, the risk of occurrence is up to four times higher.
There are two forms of the disease:
- In the dry form of AMD, there is a gradual death of retinal pigment epithelium (RPE) cells, which are responsible for the metabolism of the light-sensitive cells (rods and cones). Metabolic waste products can accumulate in this layer, forming fatty deposits (drusen).
- In the wet form of AMD, there is the formation of new blood vessels. These newly formed vessels grow into the damaged areas of the pigment epithelium. Blood and fluid accumulate, significantly reducing visual acuity. This process eventually heals with a scar, which causes a loss of central vision.
Treatment of the disease differs for each form.
In the dry form, also called atrophic, there is a loss of metabolically active cells in the retinal pigment layer and subsequent loss of photoreceptors. For treatment, it is important to take betacarotenoids – lutein and zeaxanthin, which are consumed during the visual process. Therefore, we need to supply them to the eye. With sufficient intake, the dry form can be stabilized.
Treatment of the wet form of AMD is more complex. The doctor evaluates the patient’s condition and, based on that, decides on the application of anti-VEGF injection therapy.
What is Diabetic Retinopathy?
Patients being treated for diabetes belong to the highest-risk group threatened by retinal diseases. Among the most vulnerable are young people with type 1 diabetes, who have been treated for diabetes mellitus since childhood. During their teenage years, their attention is overwhelmed by many other stimuli. They do not show symptoms and subjectively see well, so they forget about regular check-ups. These individuals are at the highest risk of vision loss. Also at risk are unsystematic patients who do not follow a dietary regimen. The condition can also be worsened by alcohol, cigarettes, hormonal contraception, or high blood pressure.
The most common disease threatening diabetic patients is known as diabetic retinopathy. As a result of high blood sugar and fat levels in the blood, microvascular occlusions form. These cause insufficient blood supply to the retina. This condition triggers the formation of new blood vessels. However, the newly formed vessels have weakened walls; their contents leak and can cause bleeding in the retina or swelling in the area of the sharpest vision. In the early stages, the patient does not feel any symptoms. Later, the newly formed vessels can cause bleeding into the vitreous, which may result in sudden deterioration or loss of vision. In the final stage, fibrous tissue forms on the retina. This tissue exerts traction on the retina, which can cause retinal detachment and thus blindness.
The key to successful treatment is:
- sufficiently early and regular retinal eye examinations,
- cooperation between the diabetologist and the ophthalmologist,
- stabilized blood sugar and blood pressure levels.
The doctor evaluates the patient’s condition and based on that selects the appropriate type of treatment: laser treatment, or treatment with corticosteroids and anti-VEGF agents. In advanced cases, surgical intervention is necessary – a procedure known as vitrectomy (PPV – Pars Plana Vitrectomy).
What are macular holes and how do they form?
Macular holes are openings or breaks in the center of the retina, in the area responsible for the sharpest vision (the macula). They form as a result of changes in the vitreous body and on the surface of the retina. Pressure inside the eye can cause the retina to stretch, which may lead to the formation of a hole.
With age, the vitreous (the gel-like substance filling the inside of the eye) undergoes changes — it becomes more liquefied, alters its structure, and gradually detaches from the retina. In some cases, this process causes a small tear in the central part of the retina, resulting in a macular hole. If a hole develops in the peripheral retina, it can lead to retinal detachment.
In certain cases (more frequently in women, partly due to hormonal changes), delicate membranes may form at the interface between the vitreous and the retina. These membranes can contract and exert traction on the retina.
Macular holes can also develop after trauma, blunt injury to the eye, or impact.
When will I notice improvement after macular hole surgery?
Improvement in vision depends on the duration and size of the macular hole—typically within a period of 1 to 9 months after the surgery. In some cases, full vision improvement may occur.
Central vision loss and, most importantly, the distortions—which are often the most disturbing symptom—are eliminated. In more severe cases, the surgery may help at least with the removal of these distortions.
In some patients, the central vision loss becomes significantly less noticeable. However, some patients may not subjectively feel an improvement. From the perspective of eye surgery, a closed macular hole is highly significant. It prevents other potential complications (such as amotio – retinal detachment, or a secondary macular hole). A macular hole is a serious retinal condition. Even minor improvement can help enhance the patient’s quality of life.
What is an Amniotic Membrane?
The amniotic membrane is obtained from the placenta, which mothers donate for medical purposes and is preserved in tissue banks. In ophthalmology, it is most commonly used in cases of eye burns, to treat corneal ulcers and defects. After surgery, no immunosuppressive treatment is needed. The amniotic membrane is a basal, body-compatible tissue that is well accepted by the body.
Can a Healthy Lifestyle Prevent Retinal Diseases?
Excessive stress is a dangerous factor in all metabolic disorders, including retinal diseases. In addition to regular monitoring of blood sugar, hemoglobin, fat metabolism, and blood pressure, doctors emphasize consistent physical activity. For diabetic patients, the rule is to try to burn as much energy as possible through active movement every day. A varied diet rich in antioxidants and avoiding smoking also has a positive effect on the retina.